Young blood can rejuvenate biological processes in aged mice, a remarkable scientific phenomenon revealed through heterochronic parabiosis. This finding challenges what we know about aging as an irreversible process. Scientists surgically join two animals of different ages to share blood circulation in this groundbreaking research technique. The approach has transformed longevity science in the last two decades.
This piece explores the science behind heterochronic parabiosis. We look at whether blood transfusion concepts like parabiosis might benefit humans someday. Let’s look to the latest scientific findings on this fascinating subject.
What is heterochronic parabiosis?
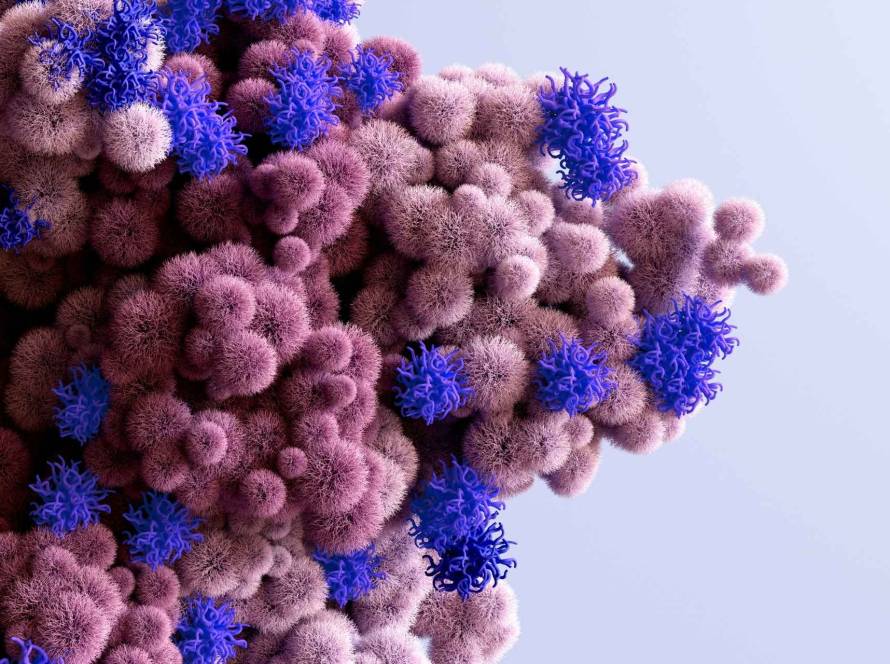
The term parabiosis comes from Greek words “para” (alongside) and “bios” (life). It describes two organisms living side by side with a shared circulatory system. Heterochronic parabiosis refers to surgically joining two animals of different ages. This creates a common blood supply that lets circulating factors flow between young and old organisms. Scientists use this method to learn about how blood borne factors affect aging processes and tissue regeneration across biological systems.
Definition and origin of the term
Parabiosis is a surgical technique that connects two living animals anatomically. The animals develop joined circulation within about a week. Scientists pair animals of different ages in the heterochronic version, usually young and old mice. They use isochronic pairs (young to- oung or old to old) as controls. The animals share blood vessels and exchange hormones, enzymes, blood cells, non-coding RNAs, extracellular vesicles and even cellular organelles.
Scientists can separate cell-autonomous from non-autonomous aging mechanisms through this technique. They study how one animal’s circulation affects its partners cellular and tissue function. The method creates two research scenarios: old animals become younger from young blood while young animals age faster from old blood.
Why it matters in aging research
Heterochronic parabiosis shows that circulating factors largely control aging. Research in the last two decades has shown that young blood can make many biological processes younger in old mice. This includes bone regrowth, hepatogenesis, myogenesis and neurogenesis.
This technique has taught us several key things about aging:
- It changes multiple signs of canonical aging hallmarks. These include altered intercellular communication, loss of proteostasis, mitochondrial dysfunction and cellular senescence;
- Scientists can identify specific blood-borne proteins. “Anti-geronic factors” make tissues younger while “pro-geronic factors” speed up aging;
- Aging doesn’t just happen because of internal cellular changes. The body’s environment plays a big role.
Heterochronic parabiosis proves that tissue aging has systemic regulation. This discovery has helped scientists find potential therapeutic targets. It has also opened new ways to develop treatments that might slow or reverse biological aging.
How heterochronic parabiosis affects aging at the cellular level
The cellular level shows fascinating insights into how aging mechanisms respond to circulating factors through heterochronic parabiosis. This procedure’s effects on cellular senescence stand out as remarkable. Senescence, a key sign of aging, stops cell growth and releases inflammatory factors.
Reduction of senescent cells in old mice
Aging and age-related diseases happen because senescent cells build up. Research shows that old mice exposed to young blood circulation have lower levels of senescent cells. The reduction shows up in many tissues, the forebrain, kidney, liver and lung of aged parabionts.
The young environment helps clear out senescent cells rather than just stopping new ones from forming. The young systemic environment actively fights against the normal age related slowdown in removing senescent cells.
Induction of senescence in young mice
Young mice paired with old partners age faster at the cellular level. Studies consistently show higher senescence markers in young heterochronic parabionts. This proves that aging factors in old blood can directly cause senescence through cell non-autonomous mechanisms.
A single blood exchange from old to young mice can trigger senescence in young animals. This happens quickly without needing long-term exposure. Many cell types feel the effects, especially satellite cells in muscle tissue. Young mice exposed to old circulation show more p16+/Pax7+ senescent satellite cells, according to studies.
Changes in SASP markers and immune clearance
Senescent cells release inflammatory factors known as the senescence-associated secretory phenotype (SASP). Heterochronic parabiosis changes SASP patterns:
- Old mice paired with young partners show fewer pro-inflammatory cytokines like IL-1β, IL-6 and TNF-α;
- MCP-1 (CCL2), which helps recruit monocytes and indicates biological aging, drops in old heterochronic parabionts;
- These changes appear in tissues of all types, which points to system-wide control of senescence.
The immune system plays a vital role here. Getting rid of senescent immune cells helps old animals immune function by stopping pro-inflammatory cytokines that cause chronic inflammation. This means heterochronic parabiosis might make aged tissue young again by fixing the immune system’s ability to spot senescent cells.
Key studies and findings
Yousefzadeh and team showed that circulating geronic factors help control senescence. Their research found that old mice in a young environment had fewer senescence markers, while young heterochronic parabionts showed more.
Studies with senolytic drugs add more proof about senescence’s role. Old animals treated with senolytics like dasatinib plus quercetin or ABT263 before blood exchange with young mice resisted the pro-geronic effects. This proves that senescent cells likely make factors that cause secondary senescence in recipient tissues.
Analysis of senescence related gene expression shows that heterochronic parabiosis affects senescence signatures in many cell types. This means changes in cellular senescence contribute to both good and bad effects of parabiosis.
Tissue-specific rejuvenation and degeneration
Heterochronic parabiosis creates remarkable changes in tissues that show how flexible aging processes can be. The shared blood system leads to patterns of rejuvenation and breakdown across organs. This gives us a chance to learn about how blood-based factors control tissue aging and renewal.
Brain: neurogenesis, endothelial function, cognition
Young blood makes big changes to aged brain vessels. Blood vessel volume goes up by 87% and branching increases by 21% in old heterochronic parabionts compared to isochronic controls. This renewal of blood vessels brings cerebral blood flow back to young animal levels. Neural stem cells then start to multiply more in the subventricular zone, which lifts olfactory neurogenesis.
Young blood fights several age related changes in the aging neurogenic niche. CCL11 levels drop, β2-microglobulin buildup decreases neuroinflammation goes down. These changes boost hippocampal synaptic plasticity and cognitive function. Old mice get better at telling different smells apart.
Muscle: satellite cell activation and repair
Muscle stem cells (satellite cells) recover well after heterochronic parabiosis. Old mice with young blood show better myogenic capacity. Their satellite cells genomic integrity comes back and muscle repair improves. Satellite cells from these old mice can form more colonies too.
Young blood changes things at the molecular level. Mitochondria look healthier, PGC1α levels go up (this protein controls mitochondrial creation) and cells clean themselves better through autophagy and mitophagy. This means heterochronic parabiosis can reverse many age related problems in muscle stem cells and tissue repair.
Liver and kidney: metabolic and structural changes
Aging livers work less well and can’t repair themselves as easily. Young blood can make old liver cells young again. The liver repairs itself faster after partial removal, DNA synthesis happens at 36 hours instead of 48 hours, according to studies. Fatty liver problems get better and the liver works more efficiently.
Kidneys also get better with young blood. Tubule and interstitial tissue scores drop in old heterochronic parabionts compared to control groups. Autophagy factors Atg5 and LC3BII increase, while P62 decreases. This suggests that cells are better at maintaining themselves.
Bone and immune system: stem cell restoration
Old animals with broken bones heal better after heterochronic parabiosis. Their ability to make bone cells comes back. Bones grow better and stem cells recover more effectively, according to studies.
The immune system improves too. The body gets better at removing old, damaged cells and other waste that builds up with age.
Translating findings to human aging and therapies
The research findings from heterochronic parabiosis in laboratory mice show promise for human applications. We have a long way to go, but we can build on this progress despite scientific and ethical challenges. Scientists are working on several treatment approaches based on the rejuvenating effects they saw in animal studies.
Senolytics and immune modulation
Senolytic drugs are another promising treatment option. These compounds target and remove senescent cells. Since heterochronic parabiosis reduces senescent cells in aged animals, senolytics might offer similar benefits without blood exchange. These drugs helped tissue repair and slowed disease progression in many animal models with age related conditions like cardiovascular disease, diabetes, kidney failure, Alzheimer’s disease and osteoarthritis.
A study suggests treating with senolytics once every two months might keep senescent cell levels much lower than without treatment. On top of that, it looks like combining senolytics with immune checkpoint inhibitors might help cancer immunotherapy work better.
Challenges in applying HP to humans
The results look encouraging, but applying heterochronic parabiosis directly to humans comes with big challenges. Joining two people’s blood systems surgically isn’t possible or ethical. While animal studies show tissue rejuvenation, the effects vary in strength and duration depending on the tissue type and test conditions.
The biggest problem is that scientists still don’t fully understand why rejuvenation happens at the molecular level. Without this knowledge, creating targeted treatments remains challenging. Scientists also need to fully explore the potential risks of systemic treatments before using them in clinics.
Current clinical research directions
Clinical research now focuses on therapeutic plasma exchange (TPE) and plasma derived products. Several ongoing trials are exploring treatments for age related conditions like Alzheimer’s disease, Parkinson’s disease, macular degeneration and recovery after joint replacement.
A breakthrough involves finding specific blood factors instead of using whole plasma. This approach could help develop more targeted treatments without needing constant plasma donations. Research suggests that umbilical cord plasma might work even better than young adult plasma at rejuvenating cells, opening up new research possibilities.
Research in heterochronic parabiosis has changed what we know about aging biology in the last two decades. Scientists once thought aging couldn’t be reversed, but now it seems remarkably adaptable and responds to systemic regulation. The evidence shows blood borne factors can significantly affect cellular senescence, stem cell function and tissue regeneration in multiple organ systems.
The trip from experimental parabiosis to potential human therapies shows how basic biological research can lead to clinical innovations. We must maintain scientific rigor and avoid rushing to commercialize, but these studies prove that biological aging might be modifiable someday.