Our original understanding of how the gut microbiome affects health has expanded dramatically. This microscopic world functions as a “hidden organ” with over 150 times more genetic informationthan the human genome itself.
This detailed piece explores the relationship between gut microbiome and disease, its importance to overall health and practical ways to support our microbial community.
How the gut microbiome impacts health?
The gut microbiome impacts health by helping with digestion, supporting the immune system and influencing mood, metabolism and inflammation. The trillions of bacteria in our gut break down food, produce nutrients and protect the lining of our intestines.
They also help train our immune system to recognize harmful invaders and reduce the risk of chronic inflammation. Some gut bacteria even produce chemicals like serotonin that affect how we feel. When the microbiome is balanced, it helps our body function well, but if it’s out of balance, it can increase the risk of digestive issues, infections, mental health problems and chronic diseases.
What is the gut microbiome?
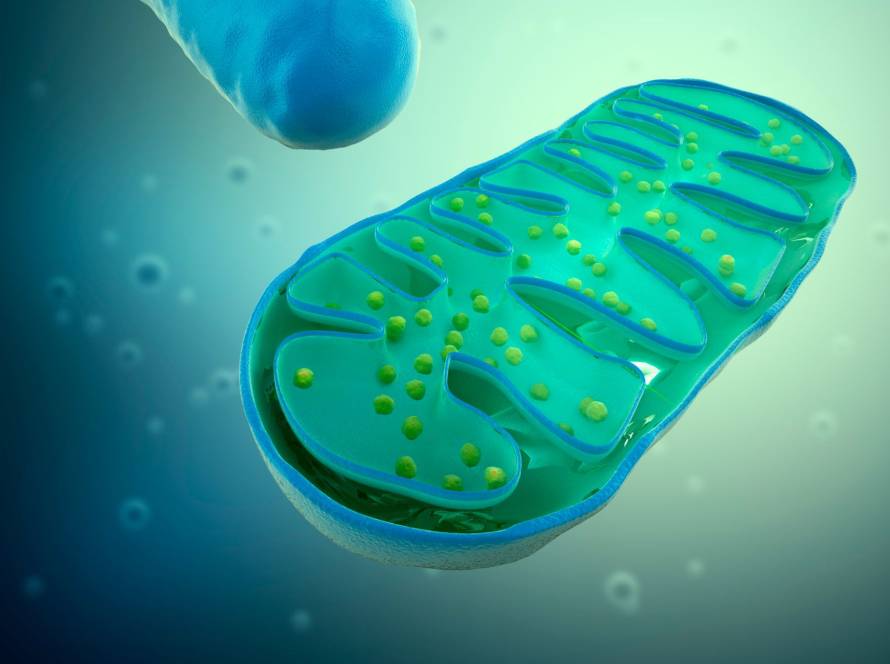
The gut microbiome is a complex ecosystem where trillions of microorganisms have evolved alongside humans for thousands of years, creating an intricate partnership that benefits both sides. This microbial community is so big that it contains approximately 10^14 microorganisms and scientists initially thought this number was 10 times greater than human cells. A new estimate suggests the ratio between human and bacterial cells is closer to 1:1.
Microbial diversity: bacteria, fungi, viruses and archaea
The human gut microbiota has bacteria, archaea, fungi and viruses. Bacteria dominate this ecosystem and scientists have studied them extensively, with four main phyla leading the pack: Firmicutes, Bacteroidetes, Actinobacteria and Proteobacteria. All but one of these bacteria come from about 30-40 species. The gut also hosts a variety of fungi like Candida, Saccharomyces, Aspergillus and Penicillium. Viruses, especially bacteriophages that target bacteria, are a vital component and might outnumber bacterial cells. On top of that, methane-producing archaea make up to 10% of all gut anaerobes, with Methanobrevibacter smithii being the most common archaeal species.
Where it lives: mostly in the large intestine
Microorganisms spread unevenly through our digestive tract. Their numbers grow steadily from the stomach through the duodenum, jejunum and ileum. The colon hosts an amazing 10¹² bacteria per gram. The large intestine holds more than 70% of our body’s microbes. This pattern exists because of different conditions along the gastrointestinal tract. Our colon creates a perfect environment for microbes with its oxygen-free space, slower flow rates and milder pH.
Why is the gut microbiome important?
Our gut microbiome works like an extra organ that provides many benefits through different body functions. These tiny organisms strengthen our gut’s defenses, extract energy from food we can’t digest and protect us from harmful bacteria. The gut bacteria are great at breaking down complex polysaccharides into short-chain fatty acids (SCFAs), which provide about 5-15% of our daily calories.
Gut microbes create essential vitamins that our body can’t produce on its own. They help transform bile acids and play a key role in developing our intestinal and overall immune system. These microbes do more than help digestion, they influence immune responses, control inflammation and even affect how our brain works through what scientists call the gut-brain axis.
Core functions of the gut microbiome
The gut microbiome does much more than just exist in our digestive tract. This microbial ecosystem acts as a powerful metabolic and immunological organ that substantially affects our overall health. It works non-stop to contribute to many physiological processes.
Digestive support and nutrient absorption
Our gut microbiome boosts our digestive abilities by breaking down compounds our bodies can’t process alone. Specific bacterial species produce specific enzymes that help ferment indigestible carbohydrates and resistant starches. The gut bacteria help metabolize bile in the intestines and support fat digestion through enterohepatic circulation. These microbes blend essential vitamins that we can’t make ourselves. Their contribution to nutrient processing gives us about 6-10% of our daily energy needs, according to studies.
Production of short-chain fatty acids (SCFAs)
The gut microbiome’s most valuable contribution comes from producing SCFAs, mainly acetate, propionate and butyrate, by fermenting dietary fiber. These compounds serve several key functions:
- Butyrate powers colonocytes and fights cancer development;
- Propionate moves to the liver, helps with gluconeogenesis and controls hunger signals;
- Acetate, the most common SCFA, flows through the bloodstream and helps peripheral tissue metabolism.
These metabolites turn on G-protein-coupled receptors, which control appetite, gut barrier function and inflammatory responses.
Immune system regulation and inflammation control
Our gut contains 70-80% of immune cells, creating a complex relationship between microbiota and immunity. Good bacteria teach our immune system to tell helpful and harmful microbes apart. Butyrate, a specific SCFA, fights inflammation by blocking pro-inflammatory pathways like NF-κB. These bacterial metabolites also strengthen our intestinal barrier by increasing tight junction proteins, which helps prevent “leaky gut” syndrome.
Neurotransmitter production and gut-brain communication
The gut microbiome’s most fascinating role might be its communication with our brain through multiple pathways. This two-way conversation happens through the vagus nerve, hormonal signals, immune mediators and bacterial metabolites. Gut bacteria shape neurotransmitter production, with intestinal cells making over 90% of our serotonin under microbial influence. On top of that, bacterial fermentation products affect the hypothalamic-pituitary-adrenal axis, which can change our stress responses, mood and cognitive function.
Gut microbiome and disease risk
New research shows that dysbiosis, imbalances in gut microbiota composition, is a vital factor in many diseases. The gut bacteria’s makeup and function affect health throughout the body in multiple ways.
Microbiome and metabolic disorders: obesity, diabetes
Dysbiosis substantially affects metabolic disorders. Studies show obese people have an increased ratio of Firmicutes to Bacteroidetes compared to lean individuals. This changed composition helps extract more energy from food and changes how fat gets stored.
People with type 2 diabetes show fewer butyrate-producing bacteria like Roseburia and Faecalibacterium prausnitzii. This reduction might explain the low-grade inflammation common in metabolic syndrome. Lean donors fecal microbiota transplants into people with metabolic syndrome showed better insulin sensitivity. These results highlight how directly the microbiome influences metabolism.
Microbiome and immune-related diseases: IBD, allergies
The gut microbiome shapes immune system development and regulation. IBD patients experience major changes in their microbial community, with less biodiversity and different bacterial composition.
Research reveals that IBD patients have fewer beneficial SCFA-producing bacteria like Faecalibacterium prausnitzii and more harmful Escherichia coli. As IBD develops, bacteria can pass through the intestinal wall more easily. This allows bacterial lipopolysaccharide (LPS) to enter the bloodstream and trigger inflammation throughout the body.
Microbiome and neurological conditions: depression, autism
The microbiota-gut-brain axis creates a two-way communication network that affects brain health. Studies show that children with autism spectrum disorder (ASD) show different gut bacteria patterns and 70% have digestive problems.
Scientists found higher levels of Clostridium bacteria in autistic children. These bacteria make neurotoxins that might cause behavioral symptoms. Depression links to higher amounts of Alistipes bacteria and fewer anti-inflammatory microbes. This suggests gut dysbiosis might lead to mood disorders through inflammatory pathways.
Microbiome and cardiovascular health
Gut microbiota affects heart disease risk in several ways. The bacterial product TMAO has emerged as a key risk factor. Studies show that higher TMAO levels link to a 4-fold increase in death risk for people with coronary artery disease. Gut bacteria change dietary nutrients with trimethylamine into TMAO, which causes inflammation and builds up plaque in arteries. However, helpful short-chain fatty acids like propionate protect the heart by lowering blood pressure through blood vessel effects.
Microbiome and cancer development
Dysbiosis leads to cancer through several pathways, especially in digestive system cancers. Research shows changed gut bacteria can cause colorectal cancer. They activate inflammatory pathways, create DNA-damaging products and disrupt normal cell function.
Certain bacteria like Fusobacterium nucleatum promote colorectal cancer growth by changing E-cadherin/β-catenin signaling. Yet some helpful bacteria make butyrate, which fights cancer by controlling cell growth and supporting the intestinal barrier.
How to support a healthy gut microbiome
Our gut microbiome needs balance and diversity through smart food choices and lifestyle habits. Scientists have found several proven ways to help good bacteria thrive in our gut.
Eat a fiber-rich, plant-based diet
Plant-based diets work wonders for our gut microbiome makeup. Research shows these diets help good bacteria flourish, especially phylum Bacteroidetes. Gut bacteria thrive on dietary fiber, with fructans and cellulose playing key roles. We’ll find fructans in onions, garlic and wheat. These compounds stay in our digestive system longer and provide lasting benefits.
Jerusalem artichokes pack an impressive fiber punch. Leeks and onions also deliver plenty of fiber. Our gut bacteria turn plant fiber into short-chain fatty acids (SCFAs). These compounds fight inflammation, support immunity and help prevent obesity.
Include fermented foods and polyphenols
Fermented foods add living microorganisms that work with our existing gut bacteria. Yogurt, kefir, sauerkraut, kimchi and raw pickles bring beneficial bacteria that can settle in our gut temporarily.
Polyphenols act as prebiotics and show up in fruits, vegetables, tea, coffee and dark chocolate. These compounds help good bacteria families like Bifidobacteriaceae and Lactobacillaceae grow while keeping harmful bacteria in check. Berries, apples, carrots and red wine boost our gut bacteria variety and antioxidant levels.
Maria Branyas Morera credited her long life to daily walks, fruit, vegetables and 3 yogurts a day:
Use of prebiotics and probiotics
Prebiotics feed our gut bacteria and can’t be digested by our body. We’ll find the main types, fructans, galacto-oligosaccharides and resistant starch, in garlic, onions, chicory and Jerusalem artichokes.
Probiotics are living beneficial microorganisms, mostly from Lactobacillus, Bifidobacterium and Streptococcus families. Food sources beat supplements because they offer extra nutrients.
Avoid unnecessary antibiotics
Antibiotics can throw our gut bacteria off balance for months after treatment. Studies show azithromycin reduces beneficial Bifidobacterium species. A high-fiber diet helps restore good bacteria during and after necessary antibiotic treatment.
Manage stress and sleep
Better sleep means more diverse gut bacteria. Scientists found that total microbiome diversity links to better sleep efficiency. People who wake up less during the night have healthier gut bacteria. What we eat affects how well our gut bacteria make substances needed for quality sleep.
The gut microbiome is much more than a group of microorganisms in our digestive tract. This complex ecosystem serves as the life-blood of human health and affects everything from simple metabolic processes to advanced brain functions. These trillions of microbial inhabitants substantially affect our overall wellbeing through multiple connected pathways.
Gut microbiome keeps showing new connections to longevity. Our knowledge of these microscopic organisms influence on aging grows with each study, offering fresh viewpoints on living longer, healthier lives. Our gut microbiota can adapt at any age, which means positive changes can improve our health. This makes microbiome care essential to any complete wellness plan.
Read more about: